Tips and Tools to Motivate Patients

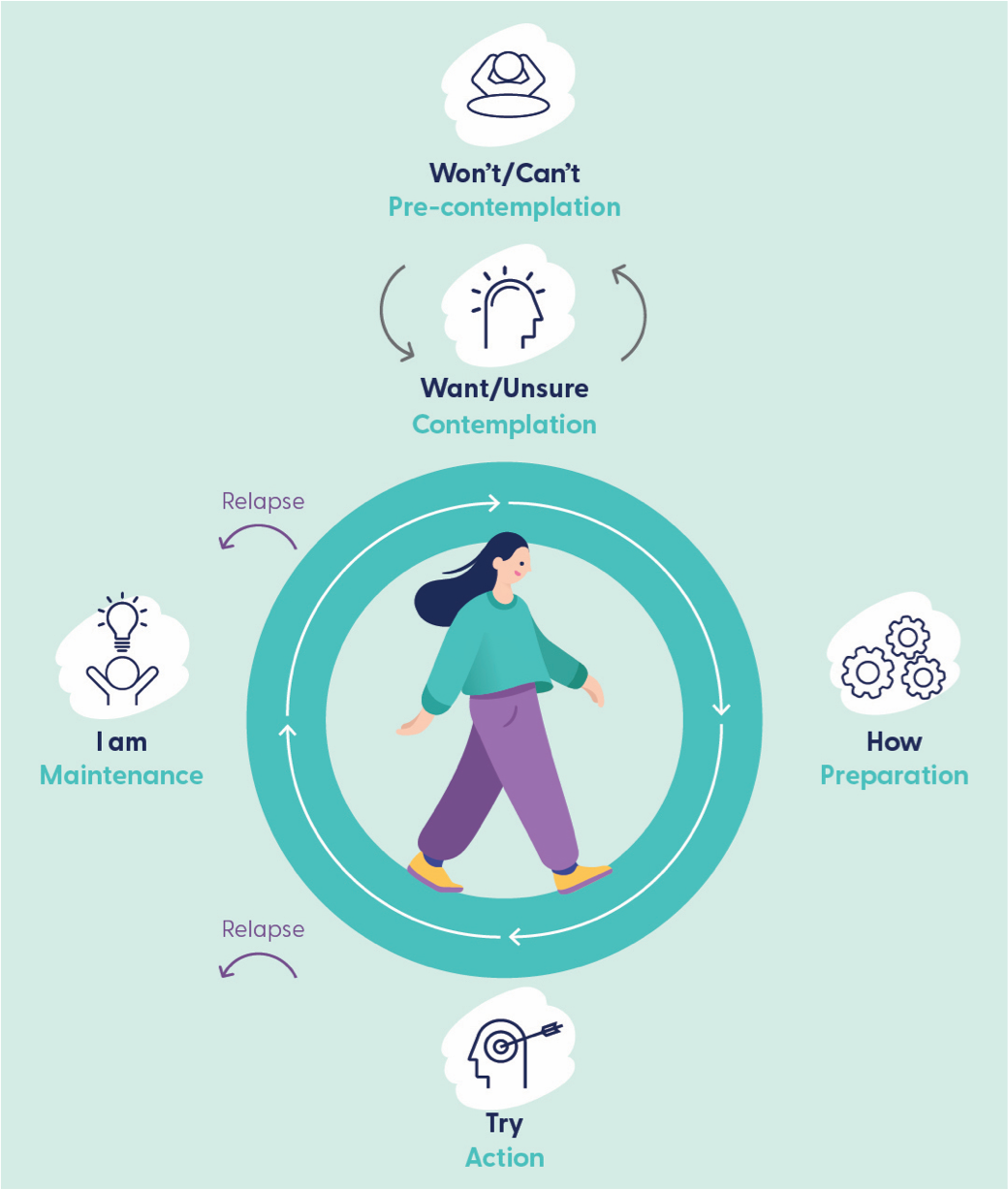
To determine the counseling required for a patient to commit to changing their physical activity, nutrition and sleep health behaviours, it is important to understand their motivation. The Behaviour Change diagram is a decision-making tool that helps identify a patient's readiness for change.
- Ask patients what lifestyle changes they could make to improve their health
- Listen to the language they use to determine their stage of behaviour change
- Click on the stage in the diagram to view and use motivational interviewing techniques tailored to their stage to support them.
The purpose of motivational interviewing is to help people find their own reasons for changing their behaviour. It is a collaborative technique that provides non-threatening opportunities to discuss sensitive issues. Scroll down to view motivational interviewing techniques and animated case studies. Explore continuing professional development offerings via the Healthy Habits Resource Hub.

Pre-contemplation
It is likely your patient is not thinking about making a change when you hear language like this: “I am happy with what I am doing” or “I can’t to do that right now.”
Conversation aim:
Spark some motivation for change.
Techniques:
Show you have heard the patient by acknowledging their thoughts and any concerns.
Raise doubt but try not to urge change.
Offer to explore the current behaviour with the patient and the benefits of changing.
Offer to provide harm reduction strategies.

Contemplation
Your patient may be thinking about making a change when you hear language like this: “I want to but” or “I think I need to.”
Conversation aim:
Strengthen motivation and develop confidence.
Techniques:
Explore ambivalence. Have the patient weigh up the pros and cons of change.
Show the patient that you understand both sides of their dilemma – the benefits and disadvantages they see in change.
Discuss possible strategies for change as “good things” and “less good things”.
Make sure your patient (not you!) has the biggest investment in the outcome.

Preparation
Your patient may be actively planning change when you hear language like this: “I know how or what to do” “I have made plans.”
Conversation aim:
Strengthen confidence and maximise readiness to change.
Techniques:
Encourage the patient to set clear but attainable goals with a realistic plan to achieve them
Reiterate the importance of starting small and working up to bigger goals.
Avoid suggesting a specific goal, they are more likely to participate when they are more invested in it than you are.
Help the patient to identify potential barriers to change and develop strategies to overcome them.

Action
You patient is likely making changes to establish a new behaviour when you hear language like this:“I am trying” or “I have just started.”
Conversation aim:
Maintenance momentum for change.
Techniques:
Review with your patient their goals to make sure they are specific:
- something that can clearly be completed
- something that can be started straight away
- related to their broader health and well-being
- set for a specific timeSupport the patient through transition.
Re-evaluate steps which are unsuccessful.
Monitor progress towards goals.

Maintenance
Your patient may have established a new behaviour and is working to maintain the behaviour when you hear language like this: “I am doing, I have done for a while.”
Conversation aim:
Bolster confidence and maintain motivation.
Techniques:
Reassure the patient that lapses are normal and not a sign of failure.
Help the patient to learn from their lapses and also from their successes.
Provide information about the difference between lapses and relapses. A lapse may be a temporary return to previous behaviour, but is not sustained over time.
Help the patient to identify and use strategies to prevent relapse.

Relapse
You may hear language from your patient that indicates they have relapsed to an earlier stage.
Conversation aim:
Build self-efficacy by reducing the sense of failure, shame and guilt.
Techniques:
Address what has which led to relapse. Avoid making any judgements as many patients fear judgement if they have relapsed or not made any progress.
Reframe the relapse from a failure to a partial or temporary success. Be curious about what they have learnt so far.
Encourage the patient that they do not have to start at the beginning again as they already know many things about how to change.
Support the patient’s belief in their motivation and ability to change.
An initiative by

In partnership with