General check-up
Select a conversation
Physical activity
Physical inactivity is the fourth leading cause of morbidity and mortality worldwide. Regular physical activity counselling by physicians is now regarded as a national health imperative. These conversation tips will help you to be more effective at supporting and encouraging your patients to improve physical activity levels and their general health.
Physical inactivity is the fourth leading cause of morbidity and mortality worldwide. Regular physical activity counselling by physicians is now regarded as a national health imperative. These conversation tips will help you to be more effective at supporting and encouraging your patients to improve physical activity levels and their general health.
Evidence
n/a
Start a conversation
Let your patient know you’re chatting about simple ways to improve physical activity, and ask if they’re interested to find out more.
Be mindful of linking patient’s current health concern with their health behaviour, it may make them resistant.
Learn more
Put patients at ease by letting them know you’re having lifestyle conversations with all your patients.
Gently gauge your patient’s interest in having the conversation to assess if they’re ready for change.
Focus on the positives from the patient’s point of view to foster a constructive, two-way conversation.
If patients aren’t interested, invite them to make a follow-up appointment when they’re ready to chat.
Evidence
BMC Family Practice
Insights
Be mindful of linking patient’s current health concern with their health behaviour, it may make them resistant.
Build well received, collaborative conversations by inviting patient’s views using a question and answer format.
Albury C, Hall A, Syed A, Ziebland S, Stokoe E, Roberts N, Webb H, & Aveyard P (2019). Communication practices for delivering health behaviour change conversations in primary care: a systematic review and thematic synthesis. BMC Family Practice, 20: 111. Link to journal article
Engage and assess
Engage your patient by asking some simple questions and assess their readiness to change. Find out how much physical activity they currently do each day.
Learn more
Assess if your patient is ready to commit to healthy changes with some simple questions.
Would you like your health to be different and, if so, how?
How do you feel about improving your physical activity?
Could you manage some small regular exercise activity, starting today?
If patients aren’t interested, invite them to make an appointment when they’re ready.
Evidence
The Physician and Sportsmedicine
Insight
Evidence supports the view today that “physicians have a responsibility to assess physical activity habits in their patients, inform them of the risk of being inactive, and provide a proper exercise prescription.”
Sallis R (2015). Exercise is medicine: a call to action for physicians to assess and prescribe exercise. The Physician and Sportsmedicine, 43(1), 22-26. Link to journal article
Understand your patient's challenges
Work together to discover challenges or barriers to exercise, by asking simple questions.
Tell me about the things that might make it hard for you to exercise.
Would your family and friends support you becoming more active?
Is there a gym or park or another safe place where you can exercise?
Are there any gender or cultural barriers to physical activities for you?
Learn more
Identify your patient’s barriers and enablers to physical activity within their social and physical environments, to support a conversation about potential strategies and improve your patient’s potential for success.
Potential barriers to physical activity might include:
Limited time, fatigue, family obligations or other competing priorities
A lack of safe paths or open spaces for activity away from traffic
Gyms or sports clubs which are too far away or too costly to join
Feeling self-conscious about being active in a public space
Cultural expectations regarding the type of activity and its location
Safety issues, especially for women exercising alone in public spaces
Potential enablers of physical activity include:
Simple and easy to use self-tracking tools like Healthy Habits to foster motivation
Friends and family to exercise with together, or to provide support and childcare
Virtual support groups to challenge, motivate and encourage adherence to goals
Evidence
The American Journal of Medicine
Insights
Research supports a multilevel approach to physical activity counselling that considers the socioecological levels, which drive differences in physical activity behaviour by geography, sex, age, and ethnic groups.
A multilevel approach can help to reduce barriers. This involves a holistic focus on assessing physical activity levels, providing advice on increasing physical activity, reaching agreement on goals, connecting patients with resources, and arranging for follow-ups.
AuYoung M, Linke SE, Pagoto S, et al. (2016). Integrating physical activity in primary care practice. The American Journal of Medicine, 129, 1022-1029. Link to journal article
Educate and engage
Start with simple, manageable and rewarding suggestions:
Your health will improve from just 10 minutes of brisk walking a day.
Learn more
Make patients more open to change by letting them know that even a small increase in their physical activity levels can improve their health and reduce their risk of disease.
Make change more achievable by reiterating the importance of starting small and working up to bigger goals.
Encourage patients that any positive changes made to their exercise routine will help, no matter how small.
Evidence
Public Health England
Insights
An additional 10 minutes of brisk walking a day is seen as achievable by adults who are currently ‘inactive’. Adults doing less than 30 minutes of physical activity per week, where the greatest health risks persist.
For currently inactive adults, evidence shows the following benefits from 10 minutes of brisk walking for 7 days: increased physical fitness, improved mood, healthier weight and a 15% reduction in risk of early death.
Being active helps to better manage many common conditions, including diabetes, depression and arthritis.
Brannan M, Varney J, Timpson C, Foster C, & Murphy M (2017). 10 minutes brisk walking each day in mid-life for health benefits and towards achieving physical activity recommendations: evidence summary. London: Public Health England. Link to journal article
Canadian Medical Association Journal
Insight
The least physically active people gain the most by becoming even a little more active on most days.
Warburton DER, Nicol, CW, & Bredin SSD (2006). Health benefits of physical activity: the evidence. Canadian Medical Association Journal, 174(6), 801-809. Link to journal article
Journal of Family Medicine and Primary Care
Insight
Brief 2 minute interventions can improve patients’ physical activity, even if sedentary or with chronic disease.
Babwah T, Roopchan, […], & Dwarika K (2018). Exercise prescriptions given by GPs to sedentary patients attending chronic disease clinics in health centres – the effect of a very brief intervention to change exercise behaviour. Journal of Family Medicine and Primary Care, 7(6), 1446-1451. Link to journal article
Encourage one small change today
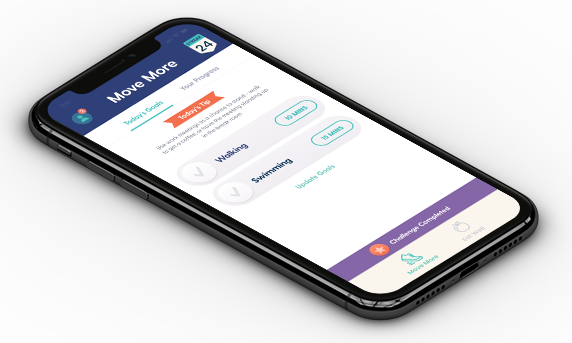
Ask patients about the activities they would like to achieve. Set a small goal and let them know they can use the Healthy Habits app to help them set, track and reach their goal. Also ask if they would like any resources printed, or a list of where to find them.
Learn more
Get an idea of your patient’s current activity level and suggest and agree on small changes to their existing levels.
Know your patient’s motivations, and work together to set achievable goals. Do they want to run 5 kilometres? Climb stairs more easily? Pick up grandkids without pain?
The Healthy Habits app is a simple and easy way to get your patients started:
It guides patients to set small, achievable physical activity and nutrition goals
Your patient can choose their own goals and increase their goals over time
The app gives your patients simple tips and tricks to help them stay on track
The Healthy Habits app allows patients to link their data to your dashboard:
You’ll be able to see how your patients have been tracking
Discuss behaviours and revise goals at their next appointment
Evidence
Annals of Family Medicine
Insight
Clinicians reported using 5 key strategies to support patient behaviour change:
Emphasising and encouraging patient ownership
Partnering with patients to identify small steps
Frequent follow-up visits to cheer successes
Listening and problem solving together
Showing caring and concern for patients
Greene J, Hibbard JH, Alvarez C, & Overton V (2016). Supporting patient behaviour change: approaches used by primary care clinicians whose patients have an increase in activation levels. Annals of Family Medicine, 14(2), 148-154. Link to journal article
Frontiers in Public Health
Insight
Self-tracking apps, which track activities like exercise, eating and heart rate, help users to better understand their health and make improvements.
Sullivan AN and Lachman ME (2017). Behavior change with fitness technology in sedentary adults: a review of the evidence for increasing physical activity. Frontiers in Public Health 4:289. Link to journal article
Journal of the National Comprehensive Cancer Network
Insight
A recent study shows that activity trackers, such as pedometers and smartphone apps, are linked to improved step counts and exercise engagement for cancer survivors.
Schaffer K et al. (2019). Systematic review of randomized controlled trials of exercise interventions using digital activity trackers in patients with cancer, Journal of the National Comprehensive Cancer Network (2019). Link to journal article
An initiative by

In partnership with